The ANC’s National Health Insurance (NHI): A Critical Examination of South Africa’s Health Care Dynamics
Introduction
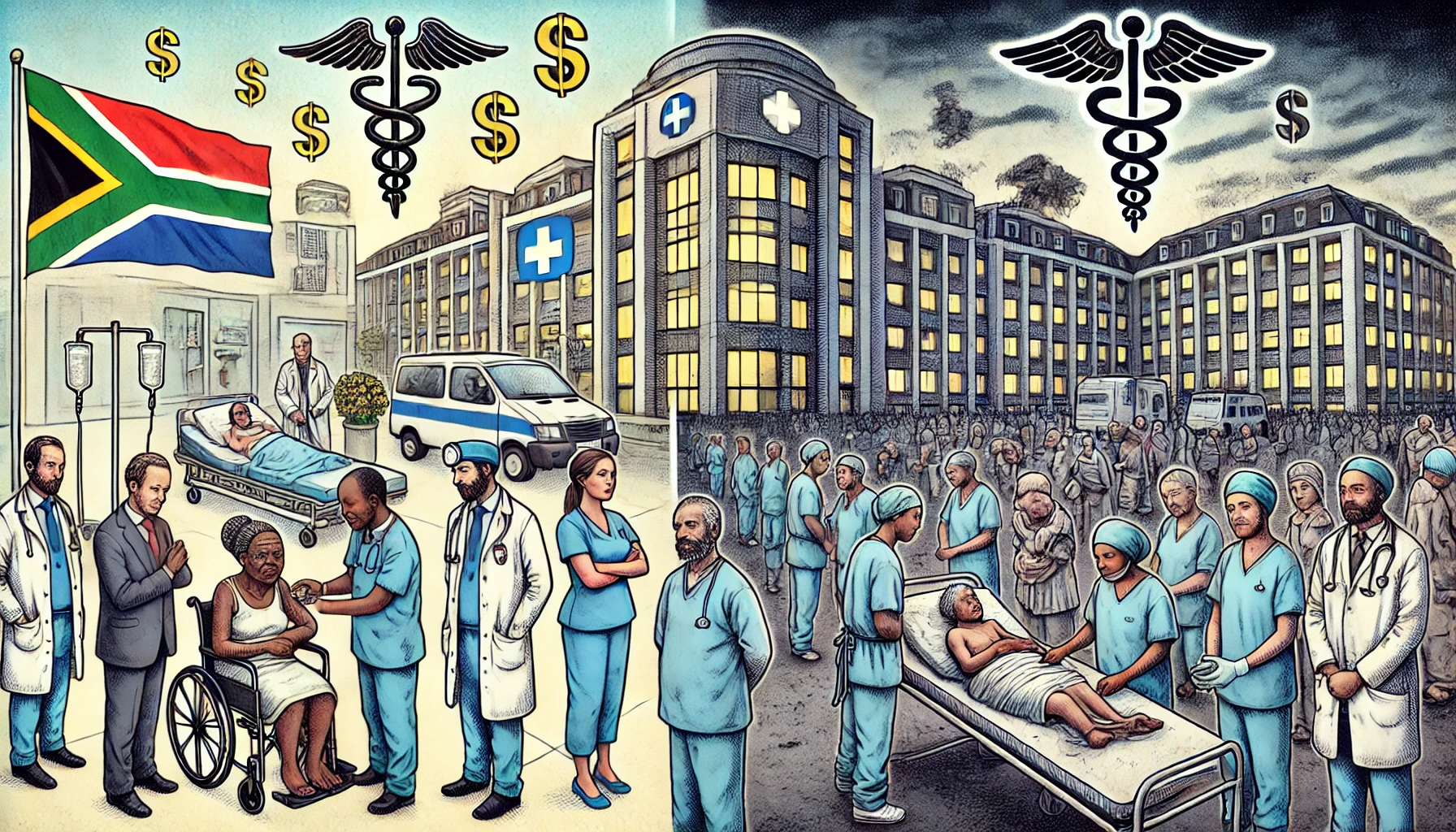
The South African healthcare system is characterized by a stark contrast between the private and public sectors. The private healthcare sector is highly commercialized, with exorbitant costs that make quality healthcare accessible only to a privileged minority. In contrast, the public healthcare sector, despite facing severe funding and staffing shortages, overcrowding, and deteriorating infrastructure, often provides care with notable levels of compassion and dedication. This dichotomy raises critical questions about equity and justice in healthcare delivery. The African National Congress (ANC)’s proposed National Health Insurance (NHI) aims to address these disparities by establishing a more equitable healthcare system. This article critically examines the NHI, the commercialization of private healthcare, and the comparative dynamics of compassion and care in both sectors.
The Commercialization of Private Healthcare
Escalating Costs and Quality of Care
The commercialization of private healthcare in South Africa has led to skyrocketing costs. Private medical institutions operate on a for-profit basis, prioritizing financial returns over patient care. This has resulted in a healthcare market where services are commodified, and patients are often treated as commercial objects rather than individuals with unique health needs (Ataguba & McIntyre, 2018). The high cost of private healthcare creates a significant barrier to access, contributing to healthcare inequities.
Impact on Compassion and Care
Despite the high costs, the level of compassion and personalized care in private healthcare institutions is frequently questioned. The profit-driven model tends to prioritize efficiency and turnover, which can compromise the patient experience. Studies have shown that in environments where healthcare delivery is heavily commercialized, the patient-provider relationship can suffer, leading to reduced levels of empathy and patient satisfaction (Gilson & Erasmus, 2019).
The Public Health Sector: Challenges and Compassion
Funding and Staffing Deficits
The public health sector in South Africa is plagued by substantial funding deficits, inadequate staffing, and crumbling infrastructure. These challenges are exacerbated by a high patient load, leading to overcrowding and long wait times for medical services (Mahlathi & Dlamini, 2017). The disparity in resources between public and private healthcare is stark, with the public sector serving the vast majority of the population with significantly fewer resources.
Compassionate Care in Adversity
Despite these challenges, the public health sector is often noted for its high levels of compassion and dedication among healthcare workers. The commitment to patient care in under-resourced settings is frequently highlighted as a strength of the public sector. This paradox of high compassion amidst resource scarcity suggests that the motivation of healthcare providers in the public sector may be driven more by a commitment to social justice and patient well-being than financial incentives (Coovadia et al., 2009).
The National Health Insurance (NHI): An Analysis
Objectives and Structure
The ANC’s NHI aims to create a unified healthcare system that provides equitable access to quality healthcare services for all South Africans, regardless of their socio-economic status. The NHI proposes a single-payer system funded through general taxes and mandatory contributions from employers and employees (Republic of South Africa, 2019). The goal is to pool resources to ensure that healthcare is based on need rather than the ability to pay.
Funding Mechanisms
The funding mechanisms for the NHI include a combination of payroll taxes, increased value-added tax (VAT), and reallocation of existing public healthcare funds. Critics argue that the proposed funding model may place an additional financial burden on taxpayers and businesses, potentially leading to economic challenges (McIntyre & Ataguba, 2012). However, proponents believe that a well-implemented NHI can achieve long-term cost savings by improving overall population health and reducing the need for expensive emergency care.
Impact on Public and Private Healthcare Sectors
The implementation of the NHI is expected to have significant impacts on both the public and private healthcare sectors. For the public sector, increased funding and resource allocation could address existing deficiencies and improve service delivery. The NHI aims to standardize care across public and private providers, potentially enhancing the quality of care in public institutions (Republic of South Africa, 2019).
In the private sector, the NHI could lead to increased regulation and oversight, potentially reducing the cost of care and improving accessibility. However, private healthcare providers may resist these changes due to potential reductions in profit margins and increased administrative burdens (Gilson & McIntyre, 2007).
Conclusion
The proposed NHI represents a critical opportunity to address the deep inequities in South Africa’s healthcare system. By examining the commercialization of private healthcare, the challenges and compassion within the public sector, and the potential impacts of the NHI, this article highlights the complexities and potential benefits of reforming healthcare delivery in South Africa. The successful implementation of the NHI will require careful consideration of funding mechanisms, stakeholder engagement, and robust regulatory frameworks to ensure that the goal of equitable, high-quality healthcare for all South Africans is achieved.
References
Ataguba, J. E., & McIntyre, D. (2018). The incidence of health financing in South Africa: findings from a recent data set. Health Economics, Policy and Law, 13(2), 103-114.
Coovadia, H., Jewkes, R., Barron, P., Sanders, D., & McIntyre, D. (2009). The health and health system of South Africa: historical roots of current public health challenges. The Lancet, 374(9692), 817-834.
Gilson, L., & Erasmus, E. (2019). Public and private health sectors in South Africa. Health Policy and Planning, 34(4), 256-262.
Gilson, L., & McIntyre, D. (2007). Post-apartheid challenges: household access and use of health services in South Africa. International Journal of Health Services, 37(4), 673-691.
Mahlathi, P., & Dlamini, J. (2017). Minimum data sets for human resources for health and the surgical workforce in South Africa’s health system. African Institute for Health and Leadership Development.
McIntyre, D., & Ataguba, J. E. (2012). Modelling the affordability and distributional implications of future health care financing options in South Africa. Health Policy and Planning, 27(suppl_1), i101-i112.
Republic of South Africa. (2019). National Health Insurance Bill. Government Gazette, 644(42598).